“The number of cancer mutations can sometimes help doctors identify the patients most likely to benefit from ICI therapy but curiously, some cancers with very few mutations can still respond very well. Our research team reasoned that these successes must be due to other immune cells that can see cancer cells even in the absence of lots of mutations.”
Co-senior author Dr Yin Wu, a Wellcome Trust Clinician Scientist at King’s College London and Honorary Consultant Medical Oncologist at Guy’s Hospital
03 January 2024
Immune cell helps predict skin cancer patients chances of responding to treatment
A type of immune cell can help predict which patients may benefit most from cancer immunotherapies, researchers from King’s College London, Guy’s and St Thomas’ Hospital Trust, and the Francis Crick Institute have found.
The study, published today in Nature Cancer, found that a rare type of T cells (a type of immune cell), can help predict the likelihood of whether a patient with advanced skin cancer will be responsive to immunotherapy treatments. The results could also lead to the development of new and more effective treatments for patients with melanoma who do not benefit from current immunotherapies.
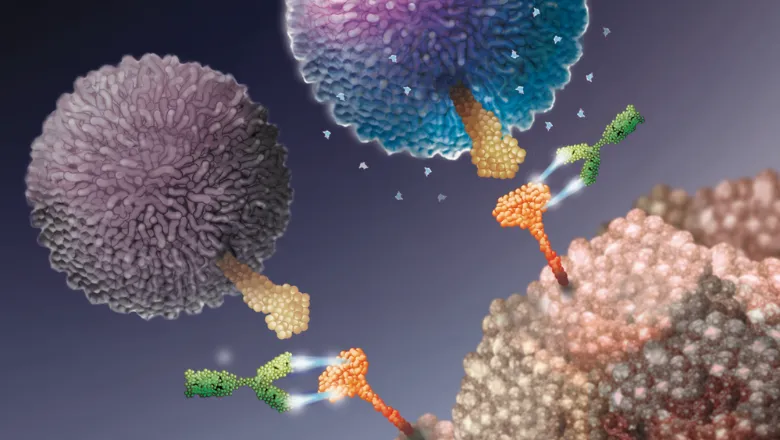
When cancer attacks the body, it can target checkpoint proteins on immune cells to weaken the body’s immune response. When this happens, the immune cells that would normally attack cancer cells are considered suppressed and ‘deactivated’, allowing cancers to grow unchecked. One type of immunotherapy treatment, known as immune checkpoint inhibitors (ICIs), can reverse this by blocking the pathways to the checkpoints on T cells.
Previous research has shown that ICIs can ‘reactivate’ T cells formerly suppressed by cancer cells. The T cells can then kill cancer cells by recognising cancer cell mutations not present in healthy cells. Where ICIs have been most successful, doctors treating cancer can seemingly cure some patients with cancer that has spread elsewhere in the body. However, this means most patients with advanced cancers do not benefit from ICIs, added to which the treatments can often cause lifelong side-effects.
A rare subset of T cells, Vd1-gd T cells, can recognise and kill cancer cells without needing them to have mutations for identification. These T cells can be found inside tumours where they also have a specific type of immune checkpoint protein, PD-1.
The researchers analysed clinical trial data from 127 patients with melanoma who were treated with ICIs that targeted the “PD-1” immune checkpoint and found that the presence of Vd1-gd T cells was highly predictive of positive responses to ICI therapy, particularly in cancers with few mutations. The team then used a new technique to isolate and grow these cells from human tissues and were able to show for the first time that the Vd1-gd T cells can be reactivated by ICI therapies currently used in the NHS to treat patients with advanced skin cancer.
Co-first author Dr Shraddha Kamdar, a Research Fellow at King’s, said: “The study findings may help doctors decide which patients are most likely to benefit from current immunotherapies. These therapies are both costly and importantly can cause severe and life-long side effects, so it is important to be able to predict when they will actually work.”
The team also found evidence that the Vd1-gd T cells could be more resistant to suppression from cancer cells compared with more common T cells, meaning that therapies using Vd1-gd T cells could work for longer periods of time.
Co-first author and PhD student Daniel Davies said: “Our study highlights the importance of understanding the contributions of lesser-studied immune cell types in efforts to improve the effectiveness immunotherapies.”
These findings may help doctors decide which cancer patients would benefit most from certain immunotherapy treatments. The ability to predict whether a patient will have a high chance of responding will save medical service providers from ordering costly treatments that may not work and help prevent patients from undergoing potentially toxic treatments that won’t help their cancer.
“Collaboration is key to any scientific study, and this project shows the benefit of working together across institutions. The study’s results are striking, and strongly support ongoing efforts to directly infuse Vd1-gd T cells into patients with cancer, an approach pioneered at King’s College London and the Francis Crick Institute.”
Co-senior author, Adrian Hayday, Professor of Immunobiology at King’s and Principal Group Leader at the Francis Crick Institute



