Surveillance in mental health wards
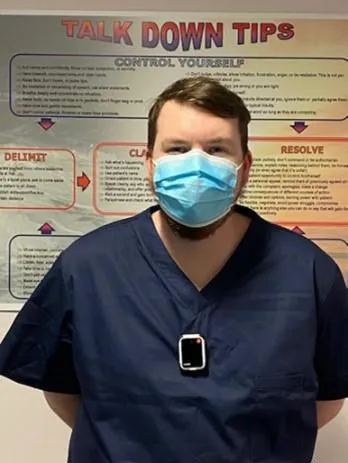
Body worn cameras (BWCs) are mobile audio and video capture devices allow the wearer to record what they see and hear. This technology is currently used by public services such as the police and increasingly within healthcare settings.
Although body worn cameras are deployed in a range of settings including a number of healthcare services, the absence of universal standards or guidelines for how they are used in these environments has raised several policy, ethical and practical concerns.
Clinicians and patients have reported strong views and have raised valid ethical concerns about the use of cameras and their potential impact on people at their most vulnerable. Within mental health hospitals, these issues include confidentiality and a lack of awareness or consent amongst patients.
Currently, there is limited availability of published evidence on the effectiveness and acceptability of body worn cameras in healthcare settings.
Our research
We have conducted some of the first and largest independent studies exploring the use of BWCs in inpatient mental health settings. These include two systematic reviews, qualitative national study, and a mixed methods evaluation of BWCs use on inpatient wards.
Systematic reviews
Our team conducted a review of BWCs use across a wide range of public and healthcare settings. We found there is limited evidence for the efficacy of BWCs as a way to control and manage violence within mental health inpatient wards. The technology has shown to be effective in reducing the number of public complaints in a law enforcement setting, but it is unclear how this is achieved. It appears there may be potential beneficial uses and unintended consequences of BWCs yet to be explored by mental health services.
In addition to this, members of our team also contributed to a systematic review of the literature on digital surveillance technologies in mental healthcare, commissioned by NHS England, undertaken by the NIHR Policy Research Unit in Mental Health.
Qualitative study
During our interview study we interviewed 33 service users and 31 health professionals across five NHS Trusts and via social media to help us understand the views and experiences of people about the use of BWCs in this setting, and to help identify the possible impact such technology might have on patients, clinicians, and the care being delivered.
The results of the study made it clear that both staff and service users were conflicted and uncertain about the use of body-worn cameras. They raised a number of important issues related to trust, power dynamics and the ethics of using this technology, namely:
- Violence and aggression are complex issues. Some staff perceived acts as deliberate whereas others might see it as an expression of distress with multiple causes or triggers.
- Both staff and patients were concerned that wearing cameras would become a substitute for good care and the use of alternative forms of prevention or de-escalation.
- Body-worn cameras will have particular implications for patients who “already feel criminalised” in an environment where staff have much greater power than patients.
- There is a lack of trust between patients and staff, that could potentially be made worse by body-worn cameras, as staff both wear and control the cameras.
Mixed Methods Evaluation
We conducted a mixed methods evaluation of the use of BWCs on inpatient mental health wards in which we aimed to evaluate the implementation of the cameras, including the impact on incidents, the acceptability to staff and patients, the sustainability of the resource use and ability to manage the use of BWCs on these wards.
Results from a mixed methods evaluation study found no clear relationship between the use of BWCs and rates or severity of incidents on either ward, with limited impact of using BWCs on levels of incidents. Qualitative findings noted mixed perceptions about the use of BWCs and highlighted the complexity of implementing such technology as a violence reduction method within a busy healthcare setting.
Furthermore, the qualitative data collected during this pilot period highlighted the potential systemic and contextual factors such as low staffing that may impact on the incident data presented. These findings suggest that BWCs have a limited impact on levels of incidents on wards, something that is likely to be largely influenced by the process of implementation as well as a range of contextual factors. As a result, it is likely that while BWCs may see successes in one hospital site this is not guaranteed for another site as such factors will have a considerable impact on efficacy, acceptability, and feasibility.
Informing policy and practice
Our research has been used to inform the position statement published in May 2023 by the Royal College of Nursing (RCN). It has also been submitted to reviews into the use of surveillance technologies being undertaken by the Care Quality Commission and NHS England.
Funding
Our qualitative study exploring the use of BWCs was funded by both The Maudsley Charity and the Florence Nightingale Faculty of Nursing, Midwifery & Palliative Care, King's College London, Research Challenge Fund 2019. Our mixed methods evaluation of BWC use was funded by The Burdett Trust of Nursing. Funders were independent of the research and did not impact findings.

