If there is a drug that a researcher wants to test on a particular patient, we can isolate those cells from the patient, place them within the hydrogel system and treat them with the drug. This way the only thing that is changing in the system is the drug and so any changes we see can be attributed to that drug.
Suzette Lust, MRC PhD student
22 June 2021
Researchers use new materials to create blood vessels in the lab to investigate how to mend them
Their material allows the researchers to create simplified tissue models to study blood vessel diseases and test drugs
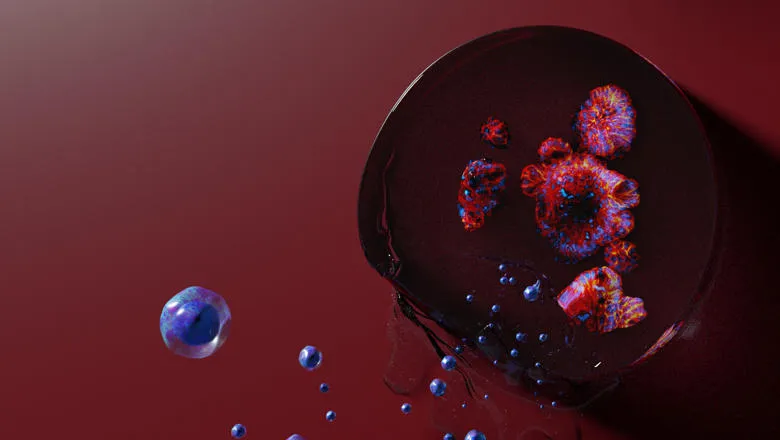
Biology and engineering researchers from King's College London have developed a novel hydrogel system, a jelly substance in which cells can be grown in 3D, to study blood vessels. The material allows them to create simplified tissue models to study blood vessel diseases and test drugs.
Their paper published today in ACS Biomaterials: Science & Engineering shows how the hydrogel created by the researchers allows the environment around the cells to be precisely changed.
The cells that live within blood vessels respond to mechanical and chemical signals from their environment. Therefore, by changing these one at a time in their hydrogels, the researchers are able to work out which cues might be causing disease.
These advances in hydrogel design may allow researchers to make personalised disease models.
By combining the hydrogels with cells taken from individual patients, it may be possible to study how disease progresses differently for each person or how they will respond to drugs.
Suzette Lust, MRC PhD student at The School of Biomedical Engineering & Imaging Sciences said instead of having to use animals to study disease, which don’t always behave like humans to study disease, hydrogels allow researchers to study human cells, within a controlled environment.
Ms Lust said the system can also address limitations with tissue samples, which can be complicated to work with and hard to get.
“Tissues can be highly complex as they include not just the cells we are interested in, but also other factors like immune cells and growth factors, which can make it difficult to understand which ones are involved in the disease and which are not.”
The team have also used their hydrogel system to study inflammatory cells in the intestine and how they contribute to inflammatory bowel disease.
They were able to show that a rare immune cell type that is abundant in the intestines of patients with Crohn’s disease may be contributing to co-morbidities like fibrosis and cancer. Their findings may have implications for developing future therapies.
Ms Lust is now using these hydrogels to make models of blood vessels to study diseases such as aneurysms, where the blood vessel wall becomes weak and can rupture.
Understanding what causes the cells of the vessel wall to weaken their surrounding tissue is crucial to help prevent these conditions from developing.
Ms Lust aims to understand whether disrupted blood flow plays a role in these diseases and to find a potential link between forces from blood flow and likelihood of developing an aneurysm.
This would allow doctors to know which patients are more likely to develop aneurysms, and treat them before they rupture.
