Our novel study can better assess fetal lung development in a range of conditions using functional MRI techniques, which we know are very safe in pregnancy. Advances in the field are evolving rapidly providing us with the ability to assess growth and development safely during pregnancy which hasn’t been previously possible in a non-invasive way.
Dr Lisa Story, NIHR Clinician Scientist and Honorary Consultant in Obstetrics and Fetal Medicine
18 October 2022
Researchers develop novel scanning methods to assess high-risk babies' lung development in-vivo
£1million Medical Research Council grant received for work looking into the use of advanced MRI techniques to evaluate fetal lung development during pregnancy

Researchers and clinicians from the School of Biomedical Engineering & Imaging Sciences have received a £1million Medical Research Council grant for work looking into the use of advanced MRI techniques to evaluate fetal lung development during pregnancy, particularly in some high-risk groups where current technology does not meet some clinical needs.
Dr Lisa Story, NIHR Clinician Scientist and Honorary Consultant in Obstetrics and Fetal Medicine and Dr Jana Hutter, UK Research & Innovation (UKRI) future leaders fellow and Professor Mary Rutherford, Professor of Perinatal Imaging, will apply a new imaging technique, combined T2*-Diffusion Imaging which allows for a simultaneous assessment of both oxygenation and perfusion of the lungs in addition to providing unique information on the tissue microstructure
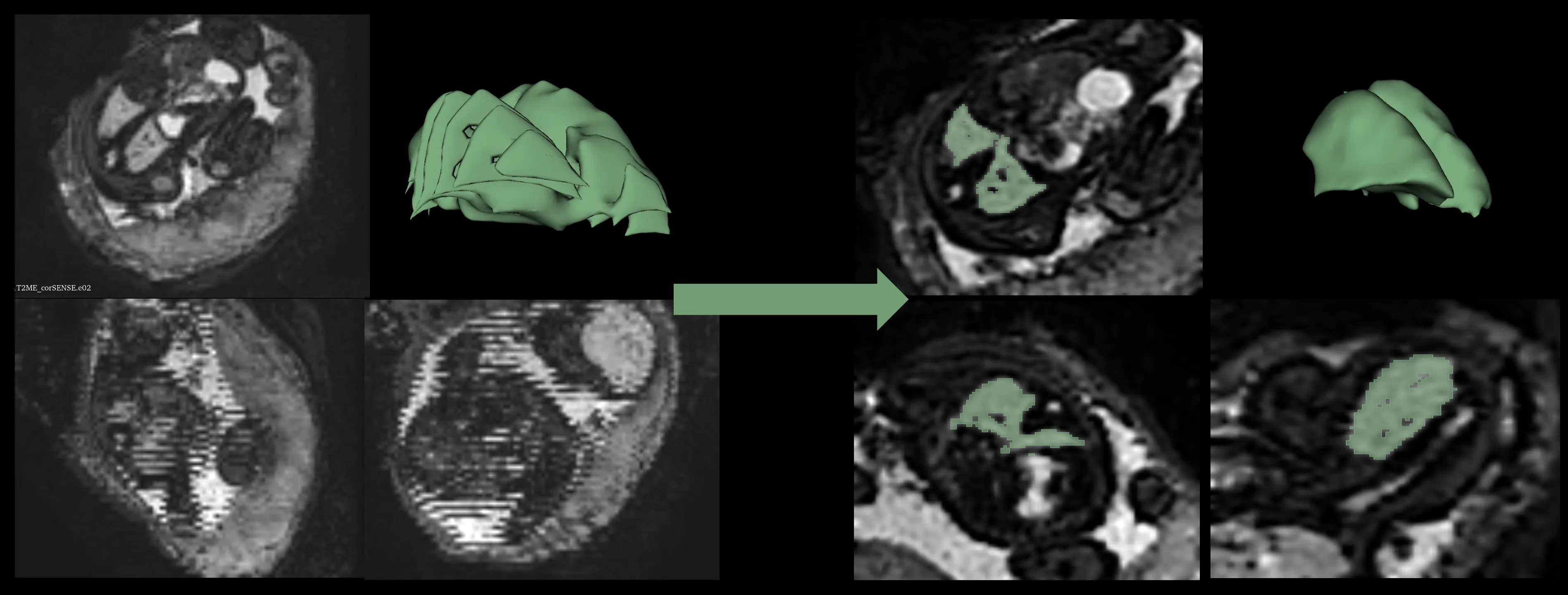
This will allow clinicians to assess the structure and function of the lungs in a much more detailed way than has been previously possible with current assessment being limited to measures of overall size. This type of information is not currently available with ultrasound.
Ultrasound is the routine approach for imaging and assessing the baby during the antenatal period and can provide some useful but more limited information in certain conditions such as congenital diaphragmatic hernia, where abdominal organs may move into the fetal chest, compromising lung development
But in other high-risk groups, ultrasound doesn’t perform quite as well in terms of predicting which babies are going to have severe problems with lung development in the future.
The study involves acquiring these MRI scans during pregnancy and women will then be invited to come back with their babies at term equivalent age. At this time point a different functional test where the baby breathes into a mask, will allow researchers to measure the volume of the lung for comparison with the antenatal MR data.
Assessment of the lungs using these new techniques will provide clinicians with much more detailed information about whether a baby will have breathing problems after delivery or indeed later in infancy and childhood and therefore will assist with parental counselling and clinical management
The researchers said in the future they might be able to identify which babies are suitable for new antenatal or postnatal therapies.
Dr Story said: “Our study will not only give information to the women and their families before pregnancy but also will enable families and their doctors to better prepare for any problems post-delivery. If you have a baby in who the lungs are very small and underdeveloped, it enables prior multidisciplinary planning to decide how best to look after the baby after birth ensuring all the relevant clinical teams are present at delivery.”



