Our findings show that overall, the campaign had no significant impact on measures of loneliness, social isolation, or levels of depressive symptoms on the over 65s. Loneliness is a common experience in older age. Approximately one in five older adults aged 65 years and old report feeling lonely across the UK and Europe, with loneliness increasingly recognised as an important public health issue. Addressing loneliness and social isolation has been incorporated in the World Health Organisation's ‘Decade of Healthy Ageing: Plan of Action 2020–2030’. However, there is limited evidence on the impact of large-scale policies and interventions on loneliness and mental well-being.
Dr Liming Li, British Academy Postdoctoral Fellow, Department of Global Health & Social Medicine
18 December 2023
England's anti-loneliness programme has no impact on loneliness, isolation, or depression amongst older people
As we head towards Christmas, a recent study shows campaign to tackle loneliness in the over-65s hasn't worked
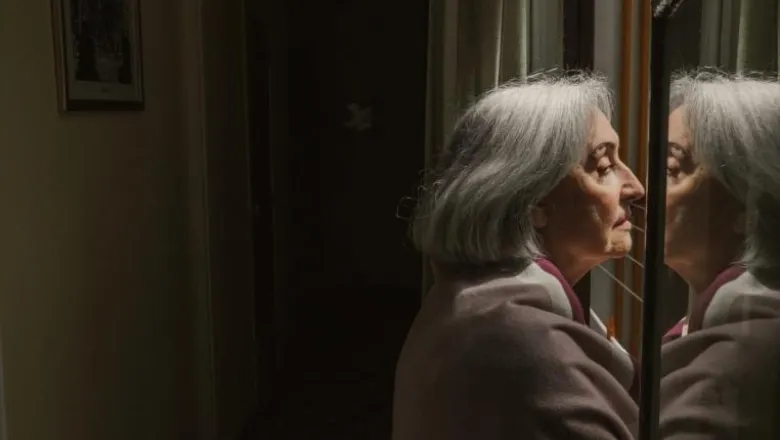
A nationwide anti-loneliness strategy has not significantly impacted loneliness or mental health in older people in England, according to a recent study.
However, the study did find that among well-educated and higher-income older adults, the campaign slightly reduced loneliness and increased social engagement.
The authors suggest combating loneliness in most older people might require longer periods of exposure, a larger scope of intervention, or more targeted strategies.
The campaign, End Loneliness, was started by a group of charities, researchers, and experts who recognised the need for a coordinated and strategic approach to tackling loneliness. Since 2013 it has operated by raising awareness and lobbying.
These actions prompted local authorities to develop a range of strategies aimed at tackling loneliness, such as improved public transport access, greater investment in support services, or organising social activities.
The paper suggests three possible reasons for the limited effects generated by these anti-loneliness strategies.
First, the intensity and level of investment in anti-loneliness activities may be too low in most local authorities and insufficient to generate change.
Second, a public campaign might operate through a complex chain of effects that involve increasing awareness and identification, followed by adoption of concrete strategies by local authorities. These changes will need to be sustained over time in order to generate impact and as a result, the UK anti-loneliness campaign might require long periods of exposure to generate measurable changes.
Third, the “structural” causes of loneliness remain and may not be altered through a public loneliness campaign, as it may relate to long-standing living arrangements, patterns of social interaction and changes in family composition, which may be difficult to change through a local authority campaign.
Major risk factors that render older people feeling lonely include age-related decline in abilities, economic hardship, loss of loved ones, and poor health.
Loneliness increases the risks of dying, with an impact comparable to physical inactivity and obesity. The lonely generally suffer poor health, cognitive impairment, and depression.
Published in the American Journal of Geriatric Psychiatry, the study looked at adults aged 65 and over who participated in either the English Longitudinal Study of Aging between 2008-2017, or between 2009-2019 as part of the UK Household Longitudinal Study.
Information from about 10,000 people was included, with the data analyzed geographically at the level of individual local authorities.
On average, one person in five reported frequent feelings of loneliness. The proportions were slightly higher in London (23%) and the Southwest (22%), while that was slightly lower in the East region (17%).
Dr Li said, in light of the study, further research is required to identify the public health or community-based interventions that may be more effective in generating changes in behavior, and which may be more effective in reducing feelings of loneliness among older people.
The exception was participation in activities such as education, sports, or arts, which increased in response to the campaign – but only among people who were educated to A-level or above. Loneliness also decreased amongst those in the top quartile of household incomes. However, these changes did not translate into significant improvement in their mental health.
Dr Li said: “One reason that accounts for the observed reductions in loneliness and increases in social participation among highly educated or high-income older people may be due to the “intellectual” nature of activities carried out as part of the anti-loneliness programmes. Another potential explanation is that highly educated or high-income individuals may have more freedom in time allocation which enables them to benefit more from an anti-loneliness campaign, compared to their peers.”



