The concern is that at the start of lockdown health systems such as in the UK suggested that some surgeries, for example bowel cancer surgery, could be safely deferred by up to 12 weeks. Our study suggests that this is not the case and could in fact increase the risk of premature death.
Professor Ajay Aggarwal, Honorary Senior Lecturer at King’s
05 November 2020
Month delay in cancer treatment can raise risk of death by 6%
People whose treatment for cancer is delayed by even one month have in many cases a 6 to 13% higher risk of dying – a risk that keeps rising the longer their treatment does not begin – research suggests.
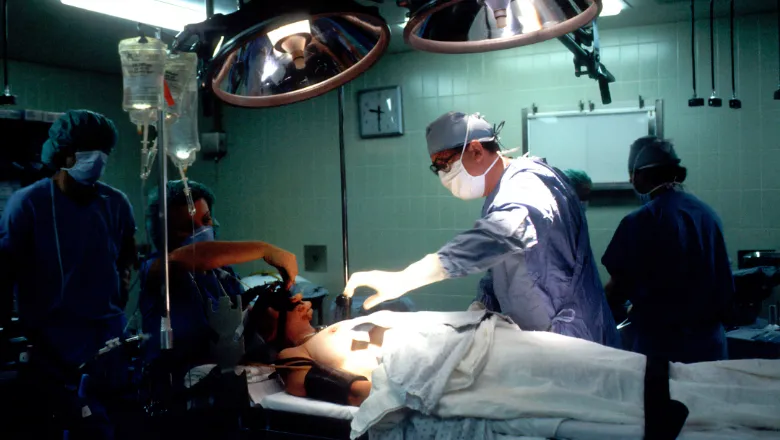
Research published today in the BMJ by an international team of researchers including King’s found there was a significant impact on a person’s mortality if their treatment was delayed, whether that be surgical, systemic therapy (such as chemotherapy), or radiotherapy for seven types of cancer.
The need for better understanding of the impact of treatment delay on cancer outcomes has come into focus during the COVID-19 pandemic because many countries have experienced deferral of elective cancer surgery and radiotherapy as well as reductions in the use of systemic therapies, while health systems have directed resources to preparing for the pandemic.
A review and analysis of relevant studies into the subject published between January 2000 and April 2020 had data on surgical interventions, systemic therapy (such as chemotherapy), or radiotherapy for seven forms of cancer – bladder, breast, colon, rectum, lung, cervix, and head and neck. Together, this represents 44% of all incident cancers globally.
Analysis of the results showed that across all three treatment approaches, a treatment delay of four weeks was associated with an increase in the risk of death.
For surgery, this was a 6-8% increase in the risk of death for every four-week treatment delay whereas the impact was even more marked for some radiotherapy and systemic indications, with a 9% and 13% increased risk of death for definitive head and neck radiotherapy and adjuvant (follow-up) systemic treatment for colorectal cancer, respectively.
In addition, the researchers calculated that delays of up to eight weeks and 12 weeks further increased the risk of death and used the example of an eight week delay in breast cancer surgery which would increase the risk of death by 17%, and a 12 week delay that would increase the risk by 26%.
A surgical delay of 12 weeks for all patients with breast cancer for a year (for example during COVID-19 lockdown and recovery) would lead to 1,400 excess deaths in the UK, 6,100 in the United States, 700 in Canada, and 500 in Australia, assuming surgery was the first treatment in 83% of cases, and mortality without delay was 12%.
The researchers used an example from the UK’s NHS, which at the beginning of the COVID-19 pandemic, created an algorithm to prioritise surgery.
A number of conditions had been considered safe to be delayed by 10 to 12 weeks with no predicted impact on outcome, including all colorectal surgery.
He added: “As we move towards the second COVID-19 wave in many countries, the results emphasize the need to prioritize cancer services including surgery, drug treatments and radiotherapy as even a 4-week delay can significantly increase the risk of cancer death. Resources need to be put in place to avoid any cancer treatment backlogs developing and elective cancer treatments must be maintained.”

