Our study reveals how genetic alterations drive cancer evolution, interfering not only with processes inside the cancer cells but also with the immune system. We can exploit this knowledge to predict who will respond to cancer immunotherapy and directly interfere with these genes to increase an immune response.”
Professor Francesca Ciccarelli, senior author of the study
09 June 2023
Uncovering cancer-immune system interactions could inform how patients respond to immunotherapy
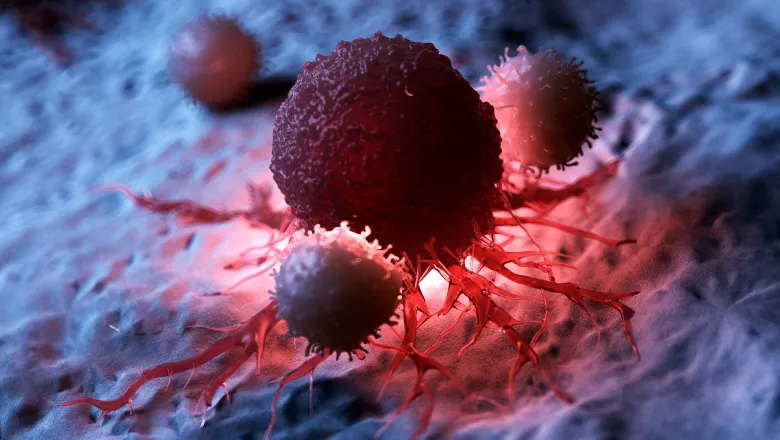
Researchers at King's College London and the Francis Crick Institute have revealed the complex interactions between cancer and the immune cells that surround a tumour, with the potential to inform how patients will respond to immunotherapy.
In the study, published in the journal Genome Medicine, the researchers analysed thousands of samples across 32 types of cancer to examine the way that cancer dynamically interacts with the tumour immune microenvironment (TIME), allowing the disease to flourish.
Cancer evolves within the TIME, which is sculpted by cancer cells and, in turn, sculpts the cancer genome. These dynamic interactions have a significant impact on how the cancer develops and responds to treatments such as immunotherapy. Gaining a greater understanding of cancer-immune system interaction is therefore crucial to understanding cancer biology.
The researchers focused on a class of genes called cancer drivers because, when altered, they help drive cancer. The researchers identified 477 of these cancer drivers that interact with multiple features of the TIME, suggesting that they drive the formation of cancer by disrupting biological processes within the cell as well as interfering with the immune system.
The study also outlined the way that two distinct classes of cancer drivers, tumour suppressors and oncogenes, operate within the TIME. Tumour suppressors are genes which when inactivated, help cancer development, whilst oncogenes need to be activated in order to promote cancer. The study revealed that alterations in tumour suppressors are prevalent in tumours with high immune infiltration (when immune cells enter the tumour), likely helping the tumour to escape the immune system. Oncogenes are instead prevalent in tumours with low immune infiltration, suggesting an opposite effect on the TIME.
As tumours with high levels of immune infiltration respond well to immunotherapy, this research shows that the burden of altered cancer drivers could be used as predictive biomarker of response to immunotherapy.
The researchers also rebuilt the entire cascade of events linking genetic alterations of specific cancer drivers to the downstream TIME modifications. They focused on head and neck cancer, a tumour type that does not respond well to immunotherapy. They developed a computational approach based on systems biology that enabled them to explain the mechanisms through which genetic drivers of head and neck cancer modify the immune system.
Our analysis uncovered links between cancer drivers and immune alterations in head and neck cancers. The mechanism driving high immune infiltration in a subset of head and neck cancers could be targeted for immunotherapy treatment.”
Hrvoje Misetic, first author of the study
The study received partial funding from the following organisations: Charles Wilson & Rowena Olegari Foundation, CRUK and the European Union.

