People with type 1 diabetes have to constantly think about their blood glucose levels and adjust their insulin doses in response. Our aspiration is to produce fully functioning beta cells suitable to implant into people living with type 1 diabetes, which do this on their behalf.”
Dr Aileen King, Reader in Integrative Physiology & Diabetes
07 December 2023
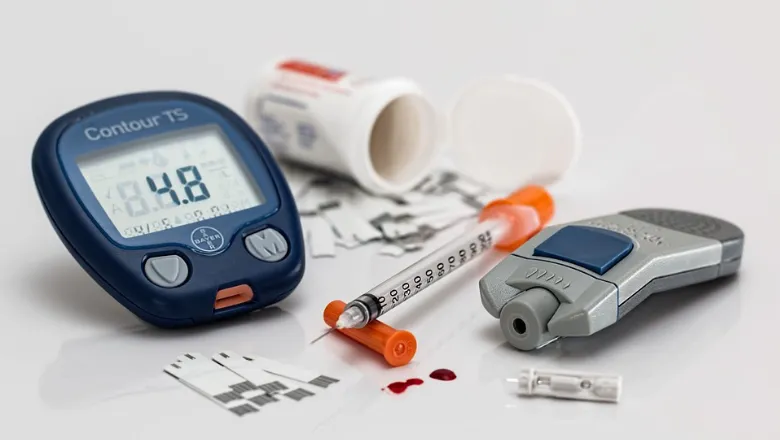
£4.8 million awarded to King's scientists to help find cure for type 1 diabetes
Two major research projects, led by Professor Shanta Persaud and Dr Aileen King, and Professor Francesca Spagnoli, Dr Rocio Sancho and Professor Molly Stevens from Oxford University, have been awarded £4.8 million funding in a bid to cure type 1 diabetes.
The two teams are among six from the UK who have received prestigious grants totalling over £13 million by the Type 1 Diabetes Grand Challenge, a groundbreaking partnership between the Steve Morgan Foundation, Diabetes UK and JDRF UK. This investment comes thanks to the historic £50 million pledge from the Steve Morgan Foundation to accelerate promising research that could unlock life-changing new treatments for type 1 diabetes.
Type 1 diabetes is an autoimmune condition that occurs when the body’s immune system attacks the insulin-producing cells of the pancreas. This means the pancreas can no longer produce insulin, leading to high blood sugar levels. More than 400,000 people in the UK are living with type 1 diabetes, including around 5,000 people in London.
The new Type 1 Diabetes Grand Challenge research led from King’s will innovate ways to restore insulin-producing beta cells that have been destroyed in people with type 1 diabetes, so the body can make its own insulin again.
Working to create an unlimited supply of elite lab-made beta cells that can deftly respond to changing blood sugar levels and are well equipped to survive transplantation will be the mission of Professor Persaud and Dr King’s team. They will utilise their team’s expertise in human beta cell development and function to innovate improved methods of turning stem cells into beta cells.
“This would be transformative for people with the condition, as it would restore the body’s minute-to-minute insulin production that is required to carefully control blood glucose levels – reducing the risk of dangerous blood sugar lows and long-term diabetes complications, while also reducing the huge psychological impact of living with diabetes,” Dr King said.
Francesca Spagnoli will co-lead another multidisciplinary team, with Rocio Sancho and Professor Molly Stevens from Oxford University, that uses human stem cells to create insulin-producing cells. These cells can be transplanted to diabetes patients, so they can synthesise insulin within their bodies.
Recent and ongoing clinical trial research has shown potential in transplanting insulin-producing cells. But the transplanted cells have a limited survival rate due to attacks from the patient’s immune system. This means that the effect struggles to last over the long term.
The project will address the causes behind the post-transplantation problems that insulin-producing cells experience. They will look at both the external environment outside of the cell, like signals between different cells and oxygen, and factors within the cells such as genes that promote cell survival.
“We envision this innovative approach to represent a substantial advancement in diabetes treatment, with the potential to positively impact the lives of millions of individuals worldwide.”
Francesca Spagnoli, Professor of Regenerative Medicine



